The Rosalie Shaw Travelling Scholarship was created in honour of our first Executive Director, Dr Rosalie Shaw, to enable APHN members from resource limited countries to attend the Asia Pacific Hospice Conference. This year, the scholarship was awarded to Yangden. She is a clinical nurse working in the palliative care unit at JDW National Referral Hospital in Thimphu, Bhutan. Below is the report of her experience at APHC 2019:
Introduction
After the 12th APHC in Singapore in 2017, Indonesia – through The Indonesian Palliative Society (MPI) –expressed their willingness to host the 13th Asia Pacific Hospice Palliative Care Conference in 2019. Indonesia understands the importance of its role in the Asia Pacific region to participate in the update of science and knowledge on palliative care.
The conference was co-organized by the Indonesian Palliative Society (MPI) and the Asia Pacific Hospice Palliative Care Network (APHN). It was attended by general practitioners and specialists, nurses, pharmacists and other healthcare workers, medical and nursing students, and volunteers involved in palliative care internationally.
It was a first for me to attend an international conference and I would like to express my gratitude to Professor Cynthia Goh and APHN for nominating and granting me the scholarship to attend this wonderful workshop. I would also like to thank my hospital for allowing me to attend the program. It was a great learning experience and a wonderful exposure for me.
Pre-Conference (1st August 2019)
We commenced the conference with a pre-conference workshop. There were 2 full day and 6 half-day workshops, out of which I attended a morning session on the Integration and Standard of Palliative Care in Clinical Oncology and an afternoon session on Comprehensive assessment of patients.
The session commenced with a presentation on the Integration of Oncology and Palliative Care by Dr David Hui of the USA. His presentation highlighted the definition of palliative care, and the physical, emotional, social, spiritual and informational needs of cancer patients. It also emphasized the importance of the role of an inter-professional team to address the holistic aspects of the needs of cancer patients through shared responsibility to achieve a common goal toward improving the quality of life of patients and their families. Different levels of palliative care and referral criteria were also presented.
The second speaker was Dr Takashi Yamaguchi from Japan and he talked on the current status of palliative care in the Asia Pacific Region and Development of Palliative Care in Japan.
There were speakers from China, Indonesia, Japan, Singapore, Taiwan and Thailand presenting on the scopes, challenges and opportunities of integrating Oncology and Palliative Care in Asian countries. They presented on the current status of palliative care, the barriers and the future opportunities in their own countries which were mostly similar. It was followed by a panel discussion on future directions on how to overcome challenges and implement integration of oncology and palliative in Asian countries.
The post lunch session was on Comprehensive Assessment of Patients and the topics covered were Breathlessness by Professor David Currow (Australia), Pain Assessment by Professor Suresh Reddy (USA), Dementia by Professor Philip Yap (Singapore) and Neurodegenerative Disorders by Professor Meera Agar (Australia).
Opening (2nd August 2019)
There was formal opening ceremony of the conference from 8:30 to 10:00 AM after the registration. The opening ceremony was chaired by the Mayor of Surabaya and the conference was officially commenced with the ringing of the gong by the Mayor.
There was a welcome message by Dr. Dradjat R. Suardi, chairman of the organizing committee, APHC, 2019. He stated, “Palliative care is a relatively new field of medicine that is not yet wildly known. Through the theme ‘Bringing Hope to Those In Despair’ for APHC 2019, it is hoped that the problems and challenges associated with palliative care development in the region can be solved through sharing of expertise and experience by world renowned experts during the conference.”
Day 1 (Friday, 2nd August)
Plenary 1 – Bringing Hope to Those in Despair: Communication in Advance Care Planning
Speaker: Professor Josephine Clayton, Australia.
She presented the framework for discussing end of life issues with patients and their families whilst facilitating hope which was followed by some practical tips for communicating about advanced care planning.
She said that as care givers, the goal is to ensure that patients are given medical care which aligns with their values, goals and preference during serious and chronic illness. She stressed on exploring the patient’s values and goals, priorities, hopes, fears and concerns for the future while assessing the patient’s or family’s readiness to discuss future care.
Plenary 2 – Palliative Care in the Last Three Days of Life: The Final Frontier
Speaker: Dr. David Hui, USA
His presentation highlighted on the progressive functional decline and worsening symptom burden experienced by cancer patients and on symptoms such as anorexia-cachexia, dysphagia and delirium which could impair oral intake. These symptoms couple with refractory cachexia contributing to persistent weight loss and decreased quality of life.
He emphasized on the need for the clinicians caring for these individuals to ensure communication about goals of care, education about natural process of time, optimization of symptom management and provide appropriate emotional support for patients and the caregivers during the last days of life.
While explaining the signs of impending death, he said, “It is important for the family members to know what to expect, planning for patient and planning for themselves. For clinicians, it is important for discharge decision, therapeutic selection of drugs and stopping of unnecessary investigations and treatments”.
After lunch programs
Scientific Session 2 – Relief from agitated delirium in the last days.
How can we maximize the use of anti-psychotics?
Speaker: Meera Agar, Australia.
What is the role of benzodiazepines?
Speaker: David Hui, USA
He talked about the importance of focusing on the humanness of medicine. He said that it is crucial to keep dying patients as comfortable and as awake as they and their families would like them to be so they can make the last few hours or days of life meaningful.
He also talked about use and effects of benzodiazepine and symptoms such as precipitate delirium, increased drowsiness, greater risks of falls and potential impact on survival. He said that benzodiazepines are like knives which are harmful if used improperly and useful if given under right circumstances.
Day 2 (Saturday, 3rd August)
There was a ‘Meet the expert’ session from 8 to 9 o’ clock. I went to meet the research expert.

Plenary 3 – Chronic Breathlessness and evidence-based update
Speaker: Professor David Currow.
Plenary 4 – Hinorara Memorial Lecture
‘Care to Count on when you’re old and Frail’
Speaker: Dr. Joanne Lynn, USA
Dr. Lynn said that we can have what we want and need when we’re old and frail but only if we deliberately build that future.
Government Authority in Palliative Care Development in Indonesia
Speaker: Official of Ministry of Health, Indonesia.
The main points of this presentation were on issues and challenges of health service in national health insurance and in Universal Health Coverage. Change in disease pattern, competency of health facility, flow of globalization, financial risk and fraud, financing quality and safety, and patient healthcare access was also discussed. He compared incidences and mortality rate of cancer worldwide and in Indonesia. The top cancers in Indonesian men were that of lung and colon and in women were cancers of the breast and cervix.
Challenges of cancer control in Indonesia were economic burden, high cost, social burden, cause of death and disability, therapy risk which are surgery, chemotherapy and radiation and multi-disciplinary involvement which were very expensive and big resources. He also talked about why hospice and palliative care started with cancer.
“You can never change things by fighting the existing reality. To change something, build a new model that makes the existing model obsolete.” Buckminster Fuller.
Scientific Session 3a – Visionary Leadership, Essential Skills for a Changing World
Speakers – Dr. Stephen Connor (USA), Professor Cynthia Goh (Singapore) , Professor David Currow (Australia), Professor Yoshiyuki Kitzawa (Japan), Professor Keiko Tamura (Japan).
After lunch programs
Scientific session 4b – Development of Hospice and Palliative Care in Asia Pacific – an APHN perspective
Speakers – Professor Cynthia Goh (Singapore), Professor Sushma Bhatnagar (India), Dr. Seema Rao (India), Speakers from Sri Lanka, Bangladesh, Myanmar and Bhutan.
In this scientific session, I had the opportunity to present on Palliative Care Development in Bhutan and the support of the Lien Collaborative in Bhutan’s journey.
There was a welcome dinner and cultural night organized by Mayor of Surabaya.
Day 3 (Sunday, 4th August)
Scientific session 5
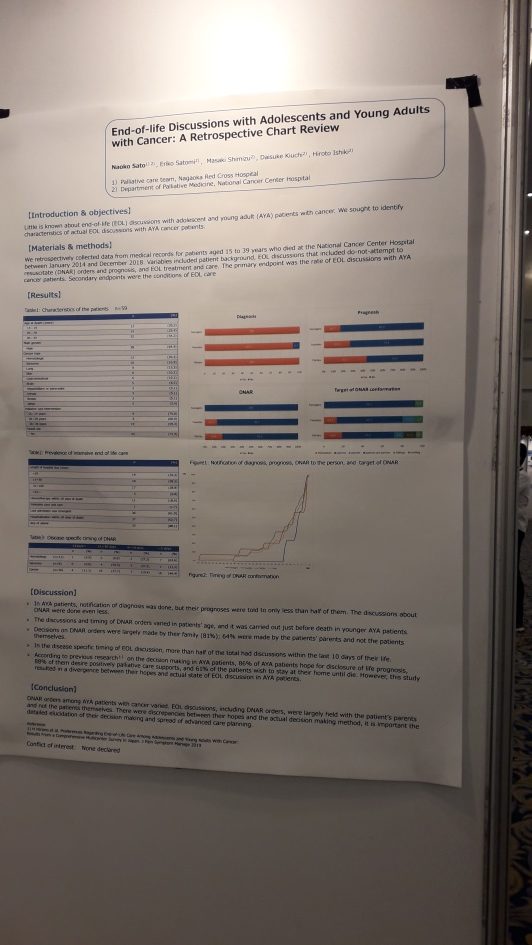
There was a session on end of life discussion and advanced care planning in Asia pacific scope, challenges and opportunities.
Speaker : Prof Josephine Clayton, (Australia) Ms. Sumytra Menon, (Singapore) Dr. Annie Kwok, (Hong Kong) Dr. Shao-Yi Cheng, (Taiwan) Dr. Hyun Sun Kim, Korea) Dr. Diah Martina, (Indonesia)
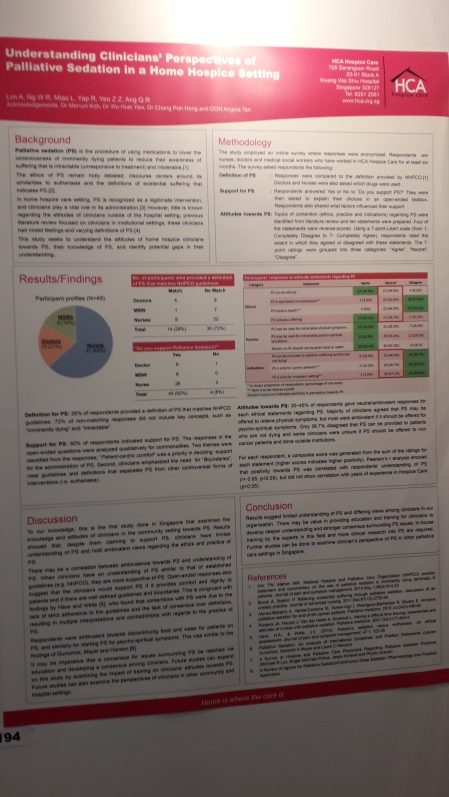
The closing ceremony was from 1:00- 3:00 PM with the exhibition of posters.
We then had the closing ceremony.
Learning Outcomes
The establishment of palliative care has not been easy anywhere. For palliative care to develop and grow, a lot of dedication, commitment, hard work and policy was necessary. Due to the wide spectrum of needs of the patients, no single discipline can provide holistic palliative care– it requires a multi-disciplinary team approach and this has been stressed time and again during the course of the conference.
Despite the treatment protocols being standardized, palliative care is a whole person care approach which is very individualized because of how the disease presents itself and how each person experiences it. In addition, education and advocacy were important factors required not only for the improvement of human resources in the field but also for the support and growth of palliative care.
Bhutan is still in the infant stage of palliative care. We have so many things to learn and a lot of room for growth and improvement. It has been educational attending the conference and getting insight on palliative care from experts around the world. We aim to develop a unique palliative care service in Bhutan by amalgamating both clinical interventions and spiritual guidance to the patients and families which aligns with our country’s developmental philosophy of Gross National Happiness.
In the near future, I am planning on conducting a session on the highlights of the 13th Asia Pacific Hospice Conference to the Palliative and Oncology Staff.
(This report has been edited by Djin Tay- APHN Volunteer Editor)