Asia Pacific Hospice Conference

Announcements
- The bid for 14th Asia Pacific Hospice Conference 2021 has been awarded to Japan.
- 13th APHC website - Abstract Submissions Open! Submission Deadline: February 28th, 2019 (UTC/GMT + 7 hrs)
13th Asia Pacific Hospice Conference, 1 - 4 August 2019, Indonesia, Surabaya
ABSTRACT SUBMISSIONS HAVE NOW CLOSED. THANK YOU.
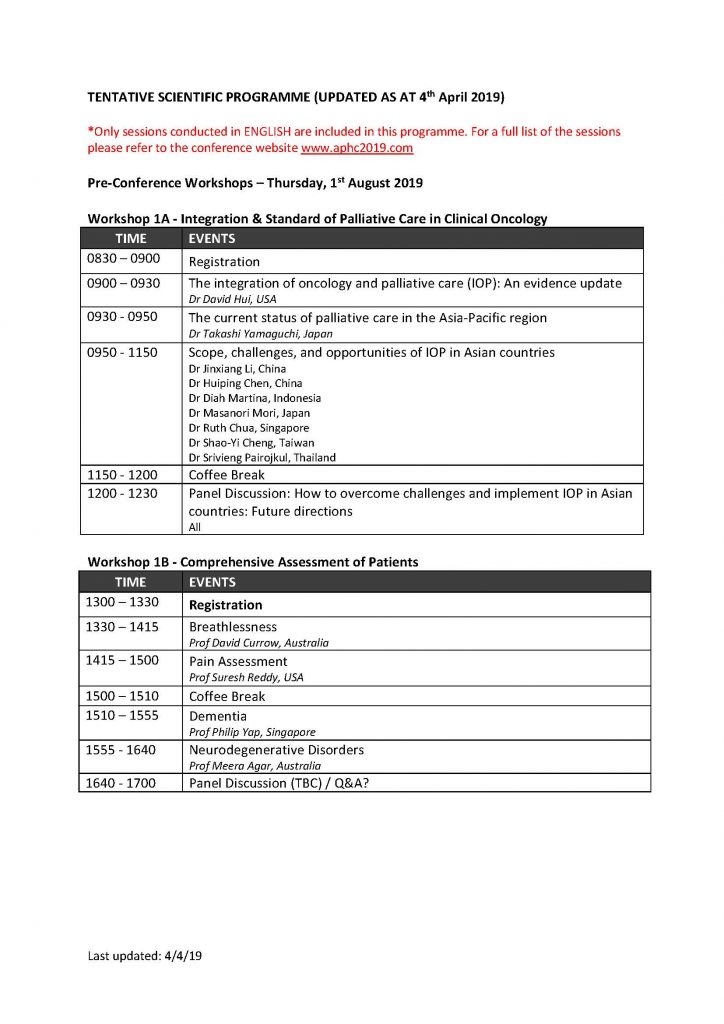
Workshop 1A - Integration & Standard of Palliative Care in Clinical Oncology
Workshop 1B - Comprehensive Assessment of Patients
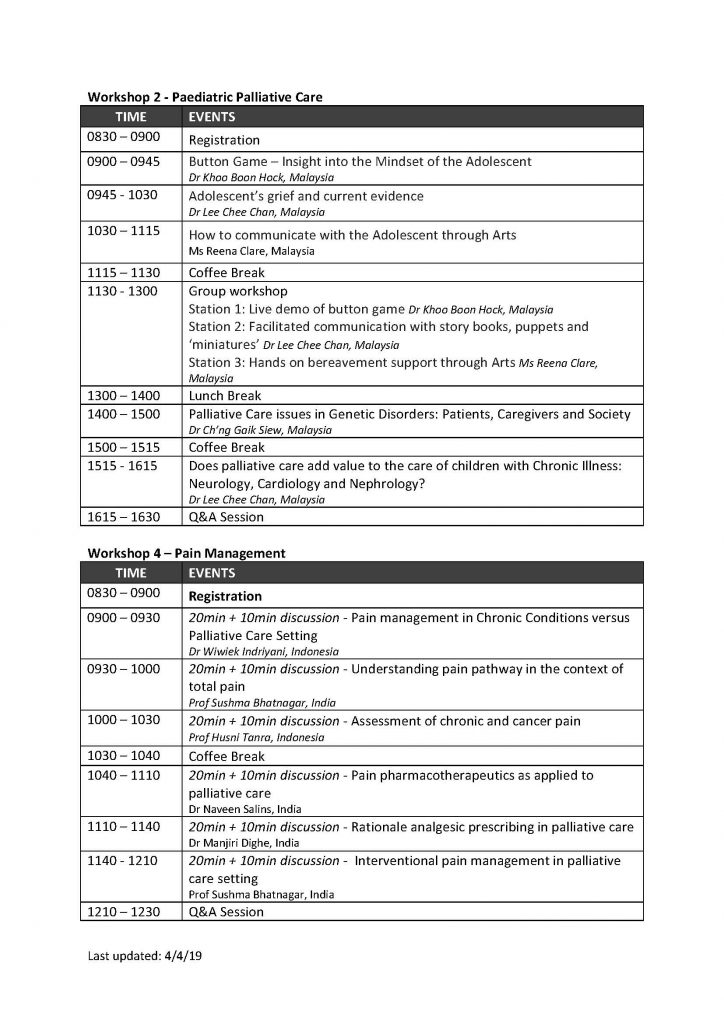
Workshop 2 - Paediatric Palliative Care
Morning session: Facilitating Ongoing Dialogues with Adolescents
9:00 – 9:45 Button Game – Insight into the Mindset of the Adolescent (by Dr Khoo Boon Hock)
9:45– 10:30 Adolescent’s grief and current evidence (by Dr Lee Chee Chan)
10:30 – 11:15 How to communicate with the Adolescent through Arts (by Ms Reena Clare)
11:15 – 11:30 Tea Break
11:30 – 13:00 Group Workshop (3 groups rotating in 3 stations, 30 minutes per station)
- Station 1: Live demo of button game (by Dr Khoo Boon Hock)
- Station 2: Facilitated communication with storybooks, puppets and ‘miniatures’ (by Dr Lee Chee Chan)
- Station 3: Hands-on bereavement support through Arts (by Ms Reena Clare)
Children with Genetic Syndromes and Chronic Illness
14:00 - 15:00 Palliative Care issues in Genetic Disorders: Patients, Caregivers and Society (by Dr Ch’ng Gaik Siew)
15:00 – 15:15 Tea Break
15:15 – 16:15 Does palliative care add value to the care of children with Chronic Illness: Neurology, Cardiology and Nephrology? (by Dr Lee Chee Chan)
16:15 – 16:30 Q & A and Feedback
 |
Dr Joanne LYNN, MD, MA, MS is the director of the Program to Improve ElderCare at the Altarum Institute. One of the first hospice physicians in the US, Dr. Lynn is author of more than 250 articles and a dozen books on palliative and end of life care. She is an elected member of the Institute of Medicine, Master in the American College of Physicians, Fellow of both the American Geriatrics Society and the Hastings Center, where she was awarded the Lifetime Achievement Award in Ethics and Life Sciences, and former faculty member of the Institute for Healthcare Improvement. Previously a medical officer for the U.S. Centers for Medicare and Medicaid (CMS), she helped craft 2010-2011 CMS reforms relating to care transitions, post-hospital, long-term care, home hospice and community settings. Dr Lynn received an MS in Evaluative Clinical Sciences from Dartmouth College, MA in Philosophy and Social Policy from George Washington Universtiry and MD at Boston University. |
 |
Dr David HUI, MD, MSc, is a tenured associate professor at the Department of Palliative Care, Rehabilitation and Integrative Medicine, with a joint appointment to the Department of General Oncology at the University of Texas MD Anderson Cancer Center, Houston, USA. His research interests include symptom management clinical trials, prognostication, integration of supportive/palliative care into oncology and research methodology. He is the principal investigator of several randomized controlled trials supported by research grants from the National Cancer Institute, the National Institute of Nursing Research and the American Cancer Society. He has authored and/or co-authored over 200 scientific papers, with his work appearing at various peer-review journals such as JAMA, J Clin Oncol, CA, Lancet Oncol and Ann Oncol. He is also the author/editor of 4 books (Approach to Internal Medicine, Drugs & Drugs, and Internal Medicine Issues in Palliative Cancer Care, 50 Palliative Care Studies Every Doctor Should Know). Dr Hui has served on several NIH grant review panels and is currently an Associate Editor of the Journal of Pain and Symptom Management. Recognized with multiple clinical, research, teaching, and leadership awards, he is a frequent speaker at various national and international meetings. In addition to academic pursuits, he remains active clinically in both palliative care and medical oncology. |
 |
Dr Marie BAKITAS, DNSc, NP-C, AOCN, ACHPN, FAAN, is Professor & Marie L. O’ Koren Endowed chair at the School of Nursing. She is also the Co-Director at Center for Palliative & Supportive Care at the University of Alabama at Birmingham (UAB). She has participated in or led over 50 clinical trials in symptom management & early palliative care. She has developed innovative methods, such as telehealth & teleconsultation, to reduce health disparities for Deep South rural & minority cancer patients & family caregivers through an implementation trial. She is also collaborating with colleagues in Turkey, Honduras, and Singapore to adapt ENABLE for these cultures. She has extended this work to advanced heart failure patients and their family via an in-progress NINR-funded R01 “ENABLE: CHF-PC: RCT of a Concurrent Heart Failure Palliative Care Intervention for Rural, Older Adults and their Caregivers”. Dr Bakitas has published over 100 original data-based papers, book chapters and books. Among her research & mentoring awards are the 2015 Friends of the NINR Path-Paver Award, 2016 HPNA Distinguished Researcher Award, the UAB Minority Health Research 2016 Charles Barkley Excellence in Mentoring Award & the Dean’s Excellence in Mentoring Award. Dr Bakitas received her ADN & BSN from the University of Bridgeport, MS in rehabilitation/oncology nursing from Boston University, post-master’s certification as an adult nurse practitioner from the University of New Hampshire, & doctoral degree (DNSc) & post-doctoral fellowship from Yale University. She is certified in Adult Health, Hospice & Palliative Care & Oncology. |
 |
Professor David CURROW, BMed, PhD, MPH, FRACP, FAChPM, FAHMS, GAICD, is a Professor of Palliative Medicine at University of Technology Sydney, the Matthew Flinders Distinguished Professor of Palliative and Supportive Care, Flinders University and Associate Director (Research) at the Wolfson Palliative Care Research Centre, University of Hull, England. Research includes clinical trials and use of large datasets to understand better the impact of life-limiting illnesses on patients and caregivers. Research into chronic breathlessness is a particular area of expertise. He is the principal investigator for the Australian national Palliative Care Clinical Studies Collaborative (PaCCSC) which has randomised more than 1850 people to phase III symptom control studies, and supports an active international phase IV collaborative with data on more than 1150 people from 11 countries. These studies have been shown to influence clinical practice. He is a foundation partner in the Australian Palliative Care Outcomes Collaborative (PCOC), an initiative to improve palliative care clinical outcomes. David has published more than 540 peer-reviewed articles, editorials and books. He is senior associate editor of Journal of Palliative Medicine and Editor of the 5th and 6th editions of the Oxford Textbook of Palliative Medicine. David is a former president of Palliative Care Australia and the Clinical Oncological Society of Australia. |
 |
Professor Josephine CLAYTON, MBBS, PhD, FRACP, FAChPM, is a Senior Staff Specialist Physician in Palliative Medicine for HammondCare’s Palliative and Supportive Care Service, based at Greenwich Hospital in Sydney and Professor of Palliative Care, Sydney Medical School, University of Sydney. She is Director of HammondCare’s Centre for Learning & Research in Palliative Care. Josephine leads a research program that aims to improve communication between patients, families and clinicians in order to enhance palliative and end-of-life care. Her research has been published extensively in leading international journals in palliative care and oncology, and widely translated into clinical practice. She also has a strong interest in teaching communication skills relevant to the care of patients with life limiting illnesses. Josephine is Director of the Advance Project, a National program funded by the Australian government ( www.theadvanceproject.com.au ). The Advance Project provides training and support for clinicians in primary care settings to initiate conversations with their patients about palliative care and advance care planning. Josephine is passionate about finding ways to help improve the palliative care of patients and their families facing an advanced progressive life limiting illness. |
Rosalie Shaw Travel Scholarship
This scholarship was created in honour of our first Executive Director, Dr Rosalie Shaw, to enable APHN members from resource limited countries to attend the Asia Pacific Hospice Conference. The successful applicant will receive support of up to USD 2,000 to fund the conference registration, travel and accommodation.
Applications will be processed through a centralised portal. The selection committee of APHN will shortlist one awardee for the scholarship and 20 awardees for the bursaries. All applicants will be considered for BOTH the Rosalie Shaw Travel Scholarship (RSTS) and APHN bursary.
Eligibility Criteria
- Must be a current individual member of APHN
- Nomination supported by 2 other APHN members
- Display leadership qualities and works in a palliative care service
- Contribution to palliative care development in your country of work or residence
- Must submit an abstract for the APHC
- Must submit a report on the benefits of attendance within 3 months after attending APHC
- Has not received any grants from APHN for the past 5 years
Preference will be given to members who have not received sponsorship of any kind for attending regional and international palliative care conferences.
APHN Bursary
What is being offered
- 20 bursaries are available
- The amount of each bursary is SGD500
- Priority will be given to participants from low/middle income countries, nurses and Allied Health workers, as well as persons who are unable to obtain other sponsorship
Eligibility Criteria
- Must be a current individual member of APHN
- Nomination supported by 2 other APHN members
- Must submit a report on the benefits of attendance within 3 months after attending APHC
- Has not received any grants from APHN for the past 5 years
- Preference will be given to members who have not received sponsorship of any kind for attending regional and international palliative care conferences.
Applications have now CLOSED, thank you for submitting your applications.
THANK YOU
Please note that this is a thank you page to thank APHN representatives for helping out in the various committees. For the complete list of committees and members, please refer to the conference website.
Chief Liaison: Dr Ramaswamy Akhileswaran
Finance Committee: Mr Fan Kwan
Co-Chair, Scientific Committee: Professor Yoshiyuki Kizawa
Members, Scientific Committee: Dr Masanori Mori, Dr Naveen Salins
Members, Abstract Review Committee:
| A/Prof Ghauri Aggarwal | Australia |
| Ms Jan Philips | Australia |
| Prof Patsy Yates | Australia |
| Dr Jane Fischer | Australia |
| Prof Magaret O Connor | Australia |
| Dr Odette Spruyt | Australia |
| Dr Anil Tandon | Australia |
| Prof Jane Philips | Australia |
| Dr Dipti Mittal | Australia |
| Dr Rico Liu | Hong Kong |
| Dr Inda Soong | Hong Kong |
| Dr Lam Wai Man | Hong Kong |
| A/Prof Amy Chow | Hong Kong |
| Dr Annie Kwok | Hong Kong |
| Prof Sushma Bhatnagar | India |
| Prof Hyun Sook Kim | Korea |
| Prof Kwon So Hi | Korea |
| Mrs Liese Groot-Alberts | New Zealand |
| Dr Sue Marsden | New Zealand |
| Dr Ross Drake | New Zealand |
| Dr Ong Wah Ying | Singapore |
| A/Prof Edward Poon | Singapore |
| Dr Gilbert Fan | Singapore |
| Dr Neo Han Yee | Singapore |
| A/Prof Lalit Krishna | Singapore |
| Dr Chong Poh Heng | Singapore |
| Dr Noreen Chan | Singapore |
| Dr Jun Hua Lee | Taiwan |
| Dr Chun Kai Fang | Taiwan |
| Prof Srivieng Pairojkul | Thailand |
| Dr Tatsuya Morita | Japan |
| Prof Tatsuo Akechi | Japan |
| Dr Jun Hamano | Japan |
| Dr Ai Oishi | Japan |
| Dr Masanori Mori | Japan |
| Asst Prof Sayaka Takenouchi | Japan |
| Dr Nobuyuki Yotani | Japan |
| Dr Ryuichi Sekine | Japan |
| Dr Isseki Maeda | Japan |
| Dr Yoshihisa Matsumoto | Japan |
| Dr Keiko Tanaka | Japan |
| Dr Takashi Yamaguchi | Japan |
| Dr Iwao Osaka | Japan |
| Dr Akira Inoue | Japan |
| Dr Harue Arao | Japan |
| Ms Megumi Kishino | Japan |
| Prof Yoshiyuki Kizawa | Japan |
Please refer to the list below for the outcome (in no particular order) of the oral presentation selection:
| ORAL PRESENTATION | ||||
| Submitting Author Name | Abstract Number | Abstract Title | Timing | |
| 1 | Lin, Chia Hui | AB19010069 | To Give or Not to Give? The Ethical Dilemma of Nursing Personnel in Care for Patients with Terminal Pancreatic Cancer: Between Pain Relief and Addiction | 11.30 – 11.45 |
| 2 | Eric Finkelstein | AB19020103 | Heart failure patients’ stated preference for aggressive end-of-life care: Does it change over time? | 11.45 – 12.00 |
| 3 | Sri Setiyarini | AB19020097 | Self-selected Individual Music Therapy to Enhance Quality of life in Palliative Cancer Patients | 12.00 – 12.15 |
| 4 | Chutchanun Ruangkhajit | AB19010082 | Development of Palliative Care Model in Home Ward, Bangkok | 12.15 - 12.30 |
| 5 | Chuang, Pei Ni | AB19020129 | Artificial hydration for the terminally ill cancer patients: A multicenter, prospective cohort study | 13.30 – 13.45 |
| 6 | Ling-Yu, Tsai | AB19010092 | The effects of team-based learning on nurses’ cognitive performance in hospice care related laws in Taiwan | 13.45 – 14.00 |
| 7 | Dr Nelfidayani | AB19030196 | Caregiver Empowerment with a Smartphone-Based Application for Geriatrics Pain Screening and Activity of Daily Living Scale | 14.30 – 14.45 |
| 8 | Martina Sinta, Kristanti | AB19030209 | The Problems and Needs in Palliative Care Caregiver questionnaire: cross-cultural adaptation for an Asian setting by a mixed method approach | 14.45 – 15.00 |
| 9 | Andy Hau Yan, Ho | AB19040211 | Family Dignity Intervention (FDI) for advancing Holistic Care in Asia Palliative Care: Preliminary Findings from a Randomized Controlled Trial | 15.00 – 15.15 |
| 10 | Yu Hsiu-Hong | AB19010086 | The Utilization of Lecture and E-learning on The Promotion of Hospice Concept to the Hospital Staff | 16.30 – 16.45 |
| 11 | Chamath Fernando | AB19010096 | Dimensions, correlates, management and perceptions related to pain among resident adult oncology patients – a Sri Lankan study | 16.45 – 17.00 |
| 12 | Takaomi, Kessoku | AB19010060 | Exploratory prospective observational study to examine the quality of life of patients who have been treated with opioid-induced constipation by using each constipation-treated drug | 17.00 – 17.15 |
Note*:
- If your name is not on the list, you will participate in the normal poster presentation.
- Participants will be contacted should there be any changes to the selection.
About the Conference
The biennial Asia Pacific Hospice Conferences of the Asia Pacific Hospice Palliative Care Network (APHN) were inaugurated in 1989 with the dual aims of enhancing our knowledge in hospice palliative care and for networking within the region.
This conference is the focal point which brings together workers, supporters and friends of hospice and palliative care in the Asia Pacific every two years.
It is the place where news is shared, new knowledge disseminated, new developments celebrated, new friendships made and old friendships renewed.
Invitation to Bid for 15th APHC
Invitation for member organizations to host the 15th Asia Pacific Hospice Conference 2023 has yet to open.
Check back for more details!
*Note: Shortlisted bids will be required to make a presentation before the council in Surabaya.
Advertising, Sponsorship and Partnership
We welcome interested individuals or organizations to collaborate with us.
Call us at +65-62355166 or Email aphn@aphn.org for a friendly chat to find out more!
Do you know?
If you are an individual member of the APHN, you will be entitled to a discounted rate at EVERY APHC!
Sign up as a member today!
Photo Gallery
This section is currently under construction. Come back later for more!
11th APHC - Taiwan, 2015
10th APHC - Bangkok, 2013

9th APHC - Penang, 2011

Previous APHCs - 1989 to 2009




































