From 5 to 9 May 2025, the Asia Pacific Hospice Palliative Care Network (APHN) conducted the fourth module of its ongoing palliative care training programme in Dili, Timor Leste. Hosted at the Hospital Nacional Guido Valadares (HNGV), the training brought together 24 committed healthcare professionals—10 doctors and 14 nurses—from across the country, representing regions including Dili, Baucau, Oecusse, Suai, Bobonaro, Ainaro, and Lautem.
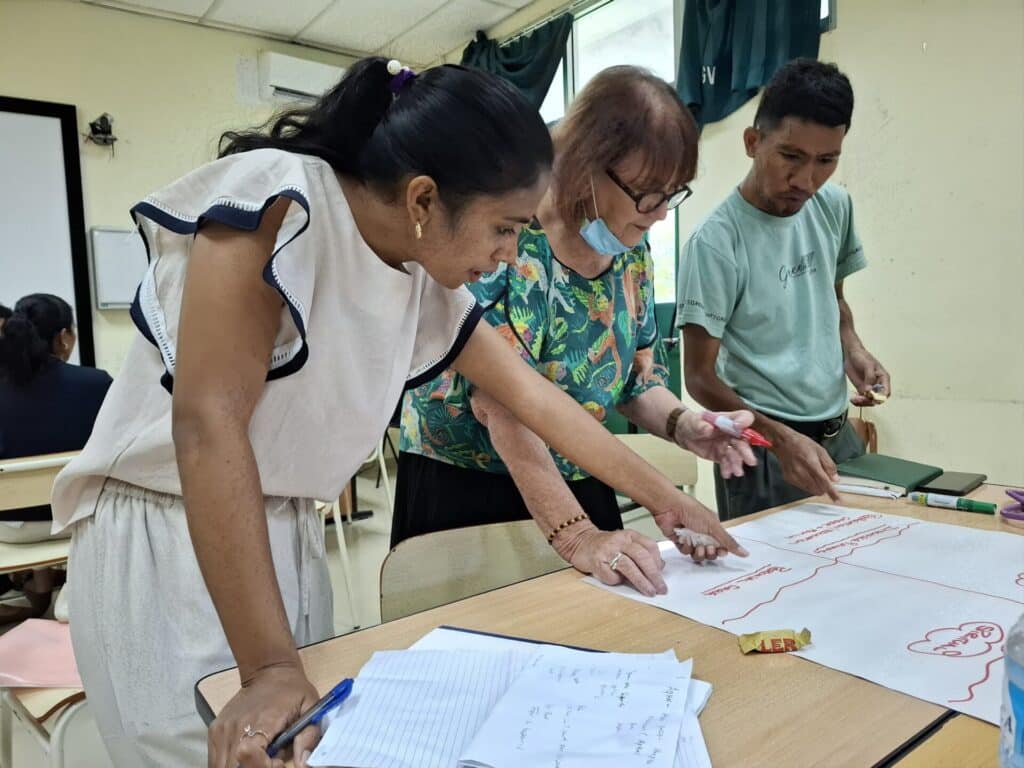
This intensive week-long programme was led by a seasoned faculty team comprising Dr Sylvia McCarthy (Malaysia), Dr Dipti Mittal (Australia), Dr Ann Toh (Singapore), and Nurse Consultants Rachel Stephen (Malaysia) and Joan Ryan (Australia). The faculty delivered a thoughtfully curated programme combining hands-on clinical training, case-based discussions, and capacity-building workshops. Participants were divided into interdisciplinary teams and rotated through structured bedside teaching sessions each morning, followed by in-depth group discussions and case presentations in the afternoons.

Institutional support for the programme was evident and deeply appreciated. The Ministry of Health was represented at the opening ceremony by Mr Carlos de Carvalho Guterres, Director of Hospital Support Services (DNASH), while HNGV’s Executive Director Dr Nuno and Clinical Director Dr Arcanjo actively supported the programme. Dr Arcanjo, in particular, emphasized the need for holistic, integrated care for palliative patients, speaking openly about the challenges of resource constraints and the necessity of engaging families in care delivery. Mr Giam, Executive Director of APHN, highlighted the mission of the network and emphasized the vital role of continuing palliative care training in Timor Leste. He stressed that by deepening their knowledge and skills through APHN’s programmes, participants could make a meaningful difference in the lives of patients facing life-limiting illnesses, offering care that is both compassionate and dignified.



There was also a significant breakthrough in engagement with the World Health Organization. While support is still developing, early conversations with regional WHO Representative, Dr Vinay and Dr Arvinc, opened the door for future collaboration and policy advocacy.

A notable highlight of Module 4 was the practical and patient-focused learning approach. Real patient cases served as the primary teaching tool, with topics spanning oral care, pain and symptom management, breathlessness, communication with families, and ethical dilemmas such as collusion and end-of-life decision-making. Several faculty members extended their teaching to include home visits, which provided additional insights into the cultural and logistical challenges of delivering palliative care in community and rural settings.





The training also encouraged the use of the Edmonton Symptom Assessment System (ESAS) and non-pharmacological management techniques for dyspnoea and fatigue, which were well received by the participants. Many reported that they had already begun applying what they learned in their respective institutions, including initiating family meetings and using communication models they learnt.



To maintain continuity and foster community, the training team used the APHN-Timor WhatsApp group that remains active. Participants have used the platform to consult on real-time patient issues, follow up after home visits, and exchange knowledge across districts. This peer-learning environment has proven invaluable in bridging geographic gaps and reinforcing a sense of shared purpose.
The week concluded with heartfelt reflections. Participants shared personal learning points, implementation strategies, and challenges they anticipate upon returning to their workplaces. Common themes included the desire to improve documentation, increase interdisciplinary collaboration, and raise awareness about the value of palliative care in non-cancer conditions. A number of participants emerged as local champions and potential future leaders—particularly among the nursing cohort—who will play an important role in sustaining the programme’s impact.
As APHN and the Lien Collaborative participants look ahead to Module 5, plans are underway to incorporate structured assessments and mentorship pathways with national stakeholders. With continued support from the Ministry of Health, WHO, and hospital leadership, the vision of accessible, compassionate palliative care for all in Timor Leste is becoming increasingly tangible.
The APHN extends its heartfelt appreciation to Deputy Minister of Health, Dr Flavio Brandão, for graciously hosting the closing dinner and reaffirming his commitment to supporting the expansion of palliative care across Timor Leste. His presence and encouragement served as a strong affirmation to both the participants and APHN of the government’s dedication to advancing compassionate care in the country.



The APHN extends its heartfelt appreciation to Deputy Minister of Health, Dr Flavio Brandão, for graciously hosting the closing dinner and reaffirming his commitment to supporting the expansion of palliative care across Timor Leste.
Written by Mr Giam Cheong Leong (APHN Executive Director )
This project is a Lien Collaborative for Palliative Care initiative to build capacity in developing countries in Asia. The Lien Collaborative for Palliative Care was co-developed by the Asia Pacific Hospice Palliative Care Network (APHN) and the Lien Foundation.
