From May 5th to 9th, 2025, I had the privilege of participating in a week-long Palliative Care Training held in Timor-Leste. This opportunity was not just a professional development experience; it was a deeply personal journey that further affirmed my commitment to advancing palliative care in our country.
What motivated me to join this training was a blend of both professional responsibility and personal conviction. As a general physician actively involved in the development of palliative care services in Timor-Leste, I am acutely aware of the suffering many patients endure due to life-limiting illnesses. Palliative care remains a relatively new concept in our healthcare system, and I have long believed that with the right knowledge and collective will, we can offer compassionate, holistic care that honors dignity at every stage of life.
Before the training began, my expectation was to deepen my understanding of core palliative care principles, particularly pain and symptom management, communication skills, and psychosocial support. I also hoped to learn how to better support patients and families emotionally and spiritually, which is often a neglected dimension of care. I am grateful to say that not only were these expectations met, they were significantly surpassed.
One of the most powerful and memorable moments of the training came during a case presentation by Dr. Andre from Sabeh. He shared the story of a 48-year-old man suffering from a chronic Marjolin ulcer, a condition that left him with a painful, foul-smelling wound. The patient was not only burdened by physical pain but also deeply stigmatized by his community and even some of his own relatives, who distanced themselves because of the odor. In response, Dr. Andre and his team of volunteers carried out community and family meetings to educate and re-engage those around the patient. With continued wound care and emotional support, the patient’s condition improved significantly, and the smell disappeared. In a profoundly moving moment, Dr. Andre brought the patient to meet us on Day 3 of the training. Seeing him in person—alive, smiling, and filled with dignity, was a powerful reminder of what compassionate, community-based palliative care can achieve.
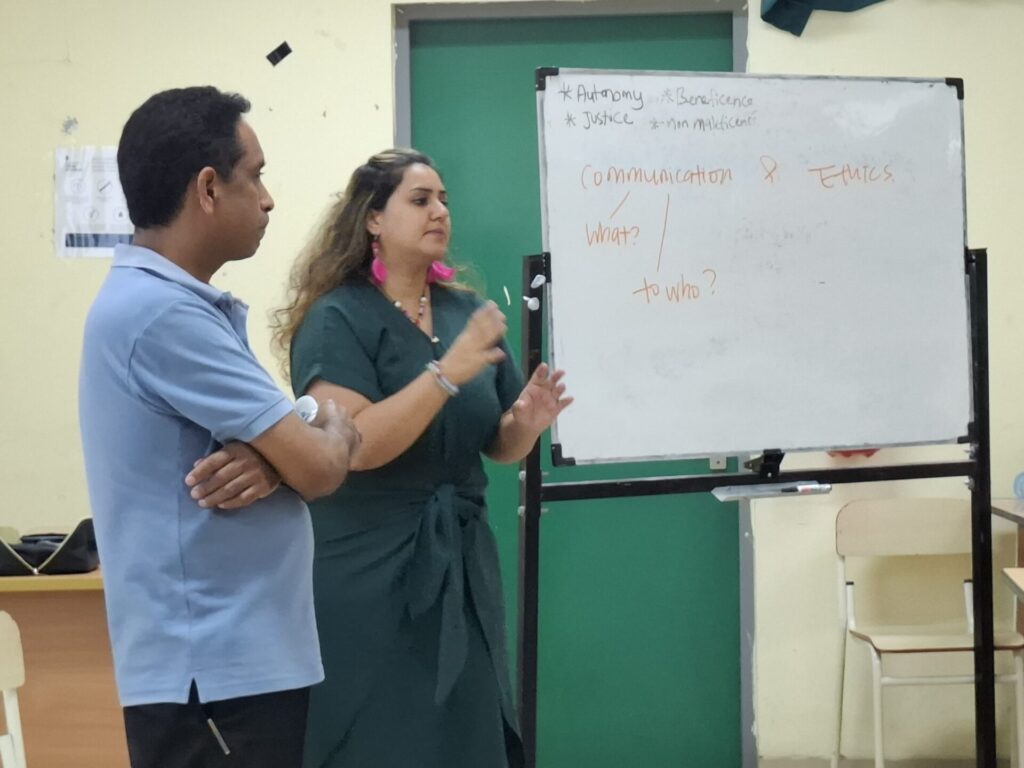
Throughout the sessions, I was especially impacted by the emphasis on patient-centered care. One session that stood out involved a role-play exercise simulating a conversation with a terminally ill patient. Although the scenario was fictional, the emotions felt real. It reminded me of a patient I had previously cared for; a middle-aged woman with metastatic cancer; whose unspoken fears and hopes I had struggled to address. The training provided practical frameworks for initiating these sensitive conversations and responding with empathy, clarity, and cultural sensitivity.
The training has deeply influenced how I view palliative care, not just as a medical intervention, but as a compassionate, person-centered approach that addresses the whole person: body, mind, and spirit.
It reinforced the idea that care doesn’t end when patients leave the hospital; in fact, for many, that’s when the greatest need begins.
At Maubisse Referral Hospital, we don’t yet have a dedicated palliative care unit. But this training has inspired me to take action in my own way. I plan to voluntarily conduct home visits for patients who are living with chronic or terminal illnesses, particularly those discharged with cancer or other life-limiting conditions. In the past, I’ve regularly called patients or their family members to check on their well-being and offer emotional support. These small acts of connection may seem simple, but they often mean the world to someone facing the end of life. I believe that even without a formal structure, we can still practice the essence of palliative care: being present, listening, and showing compassion.
Of course, we face real challenges like limited resources, lack of opioids for effective pain management, and a need for more trained personnel. But I believe that with ongoing support from networks like APHN, and by continuing to build a community of practice here in Timor-Leste, we can make meaningful progress.
My hope is that palliative care becomes integrated into every level of our health system, available in hospitals, clinics, and even in homes. I dream of a future where no one has to face serious illness or death in pain, isolation, or fear. I believe this is possible, and I am committed to playing my part.
This training reaffirmed my belief that change is not only necessary, it is achievable. It begins with each of us choosing to show up with empathy, courage, and the willingness to care. I am proud to walk this path alongside so many inspiring colleagues.
Written by Isidoro de Sousa, MD,
Hospital Referral de Maubisse, Ainaro
