EPEC Pediatrics Symposium 2023
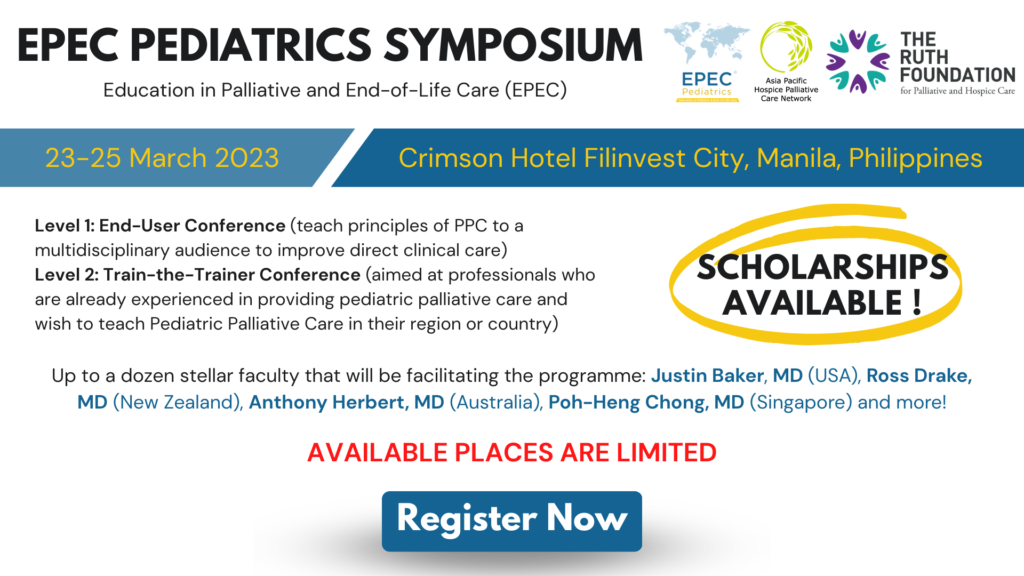
Date & Time
23 March, 2023 - 25 March, 2023
Thank you for your interest in our EPEC Pediatrics Symposium 2023! Due to the overwhelming response, the symposium has been oversubscribed and we will unfortunately not be accepting any more applications.
You can join us at our next EPEC event at the upcoming 15th Asia Pacific Hospice Palliative Care Conference in Incheon, Korea for the EPEC Pre-Conference Workshop! Head to our official conference website to register or for more information: http://aphc2023.kr/
About
The curriculum features evidenced-based knowledge in pain and symptom management and state-of-the-art training in critical clinical skills required to address key domains in pediatric palliative care.
This customised edition is facilitated by a strong international faculty who are leaders in PPC. It offers many precious opportunities to meet invited experts in small classroom sessions with high teacher-student ratios.
Stratified at two levels of practice (End-User and ‘Train-the-Trainer’), both symposia are designed to give all types of pediatric healthcare professionals (incl. physicians, nurses, psychologists, etc) core takeaways.
End-User Conference
Date: 24-25 March 2023
Open to healthcare professionals seeking to build a robust foundation in PPC for quality care of children with serious illness (cancer or non-cancer) and their families. Topics are comprehensive and transdisciplinary, covering issues across biomedical and psychosocial domains.
To expand outreach and enrich exchange, generous scholarships are provided. See eligibility below.
Registration Fees:
Developing Regions
(a) Doctors: USD 350
(b) Non-doctors: USD 170
Developed Regions
(c) Doctors: USD 550
(d) Non-doctors: USD 400
Train-the-Trainer Conference
Date: 23-24 March 2023
Aimed at professionals already experienced in providing pediatric palliative care and who wish to advance their teaching skills further. Registrants should preferably have attended EPEC training previously (face-to-face or online) and are regularly conducting talks within their own practice.
Given that places are limited, all registrants would be subjected to shortlisting by the TtT faculty.
Registration Fees:
Developing Regions
(a) Doctors: USD 500
(b) Non-doctors: USD 300
Developed Regions
(c) Doctors: USD 800
(d) Non-doctors: USD 500
Please take note:
Developing Regions: Low-income economies and Lower-middle income economies*
Developed Regions: Upper-middle income economies and High income economies*
*According to the World Bank categorisation
REGISTER HERE: https://aphn.org/epec-pediatrics-symposium-2023-registration/ (Due to the overwhelming response, we will not be accepting any more applications. Thank you.)
Faculty
 |
Justin N. Baker, MD
As a pediatric oncologist, palliative care physician, and patient-reported outcomes and Phase I and end-of-life care clinical investigator at St. Jude Children’s Research Hospital, Dr Baker is intimately aware of the distress experienced by children with advanced cancer and the communication and end-of-life/bereavement issues surrounding their disease progression. Dr Baker currently serves as the Chief of the Division of Quality of Life and Palliative Care at St. Jude. He was a founding team member of the Quality of Life for All (QOLA) Service – the St. Jude palliative care team. Additionally, he founded and continues to lead the St Jude Bereaved Parent Steering Council and Bereaved Parent Mentoring Program. |
 |
Andrea Cuviello, MD
Dr. Cuviello completed her medical degree at the University of Medicine and Health Sciences in the tropical St. Kitts and Nevis. She went on to pursue Pediatric residency training at Sinai Hospital followed by fellowships in Pediatric Hematology/Oncology at Johns Hopkins/National Institutes of Health and Hospice and Palliative Medicine at the University of Tennessee Health Sciences. After completion of training, Dr. Cuviello joined the faculty at St. Jude Children’s Research Hospital in the Divisions of Oncology and Quality of Life, providing wholistic clinical care to patients and families with life-threatening illnesses. On an academic stage, Dr. Cuviello’s work focuses on early integration of palliative care for vulnerable patient populations. She has several first author publications, highlighting palliative care needs in patients enrolling on early phase clinical trials and the use of palliative sedation therapy at the end of life, and has been invited to present at numerous national and international conferences. Currently, she is working with international collaborators in the Asia Pacific region to identify palliative care perspectives, knowledge and gaps in low- and middle-income countries. |
 |
Ross Drake, MD
Ross Drake is a Paediatrician who specialises in Pain Medicine and Palliative Care for children having gained fellowships in Paediatrics (2000), Palliative Medicine (2003) and Pain Medicine (2011) after he completed specialist training at Great Ormond Street Hospital in London and The Children’s Hospital at Westmead in Sydney. Ross is Clinical Lead of the Paediatric Palliative Care and Complex Pain Services at Starship Children’s Hospital; both being the only services of their type in New Zealand. Amongst his clinical duties he strives to improve the recognition and support of children and their families requiring palliative care or management of chronic pain. He remains very involved in developing a national approach to both disciplines and works to improve and enable equitable access and service delivery for all New Zealand children in need. Dr Drake regularly presents and teaches on children’s pain medicine and palliative care. More recently, he has been involved with establishing an international pharmacovigilance research collaborative looking at the effectiveness and adverse effects of medications and other interventions commonly used in palliative care and pain management. |
 |
Gemma Aburn, RN, PhD
Dr. Gemma Aburn is a Nurse Specialist in children’s palliative care at Starship Child Health in Auckland, New Zealand. Gemma also holds an academic appointment at the University of Auckland in the School of Nursing. She has recently completed her PhD in Nursing, exploring staff experiences of working in a children’s blood and cancer centre in Aotearoa, with a particular focus on how staff maintain resilience. Gemma established and leads the Child & Youth Health Nursing Network in the School of Nursing at the University of Auckland. Gemma is actively involved in education throughout the continuum of undergraduate, postgraduate and professional development of health professionals working with children with serious illness. Gemma is currently leading an Auckland Medical Research Foundation funded project exploring paediatric clinician’s attitudes, knowledge and skills in caring for children with serious illness and palliative care needs. This project also seeks to develop an evidence based and culturally safe education programme specific to the New Zealand context recognising care needs of both Māori and non-Māori children and their whānau. |
 |
Anthony Herbert, MD
Dr Anthony Herbert is Director of the Paediatric Palliative Care Service at the Queensland Children’s Hospital in Brisbane. He undertakes research at the Queensland University of Technology in the areas of communication, health services and medicinal cannabis. He is also project lead for the Quality of Care Collaborative of Australia for paediatric palliative care education. |
 |
Suzanne Momber, RN
Suzanne has extensive experience over 30 years at Perth Children’s Hospital in the area of Paediatric Oncology and Palliative Care within Oncology. The last 18 years she has had the role of Clinical Nurse Specialist overseeing care of children diagnosed with brain tumours, solid tumours and coordinating care for those in Oncology who require palliative care. She continues to work nationally and internationally alongside colleagues through Paediatric Palliative Care Australia New Zealand (PaPCANZ) and as facilitator of the quality of care collaboration in paediatric palliative care – QuoCCA Project in Western Australia whereby a Nurse Educator is employed to develop and provide palliative care education to health professionals statewide. In 2016 Suzanne was a finalist in the Western Australian Nursing and Midwifery Awards (WANMEA) in the category of Excellence in Leadership. |
 |
Lee-Ai Chong, MD
Lee Ai currently heads the Paediatric Pain and Palliative Care Unit at University Malaya Medical Centre in Kuala Lumpur, Malaysia. She had started there as a Paediatric Oncologist and in 2011, she decided that Paediatric Palliative Care needed more attention in Malaysia. Since then she has worked at Hospis Malaysia, a palliative care provider in the community and at the Palliative Care Unit at the Children’s Hospital at Westmead, Sydney, Australia. Her interest are also in clinical eth-ics. Her hopes are for all Malaysian children and families with palliative needs to be able to receive quality care promptly and routinely. |
 |
Poh-Heng Chong, MD
Dr Poh-Heng Chong is Medical Director of HCA Hospice Limited, Singapore and Vice Chair of the Singapore Hospice Council. He is dually trained in adult and paediatric palliative medicine. His research areas include health service design and evaluation as well as holistic care of children and young adults with life shortening illness. |
Topics
- Principles of Pediatric Palliative Care
- Pain Management in PPC
- Care of the Imminently Dying child
- Communication pearls, and ethical issues
- Goals of Care and Advance Care Planning
- Self-Care for Professionals
- Spirituality, Grief and Bereavement
- Opioid Rotation, neuropathic pain & adjuvants
- Management of Neurological Symptoms
- Management of Gastrointestinal symptoms
- Management of Respiratory symptoms
- Emotional & Behavioural Symptoms
Scholarship Application (Applications has closed on 18 February 2023)
Award recipients will receive:
- Airfare (economy class)
- Hotel Accommodation (for 3 nights)
- Registration Fee discounts
Note: Only participants from developing regions are eligible to apply.
REGISTER FOR THE SYMPOSIUM HERE: https://aphn.org/epec-pediatrics-symposium-2023-registration/
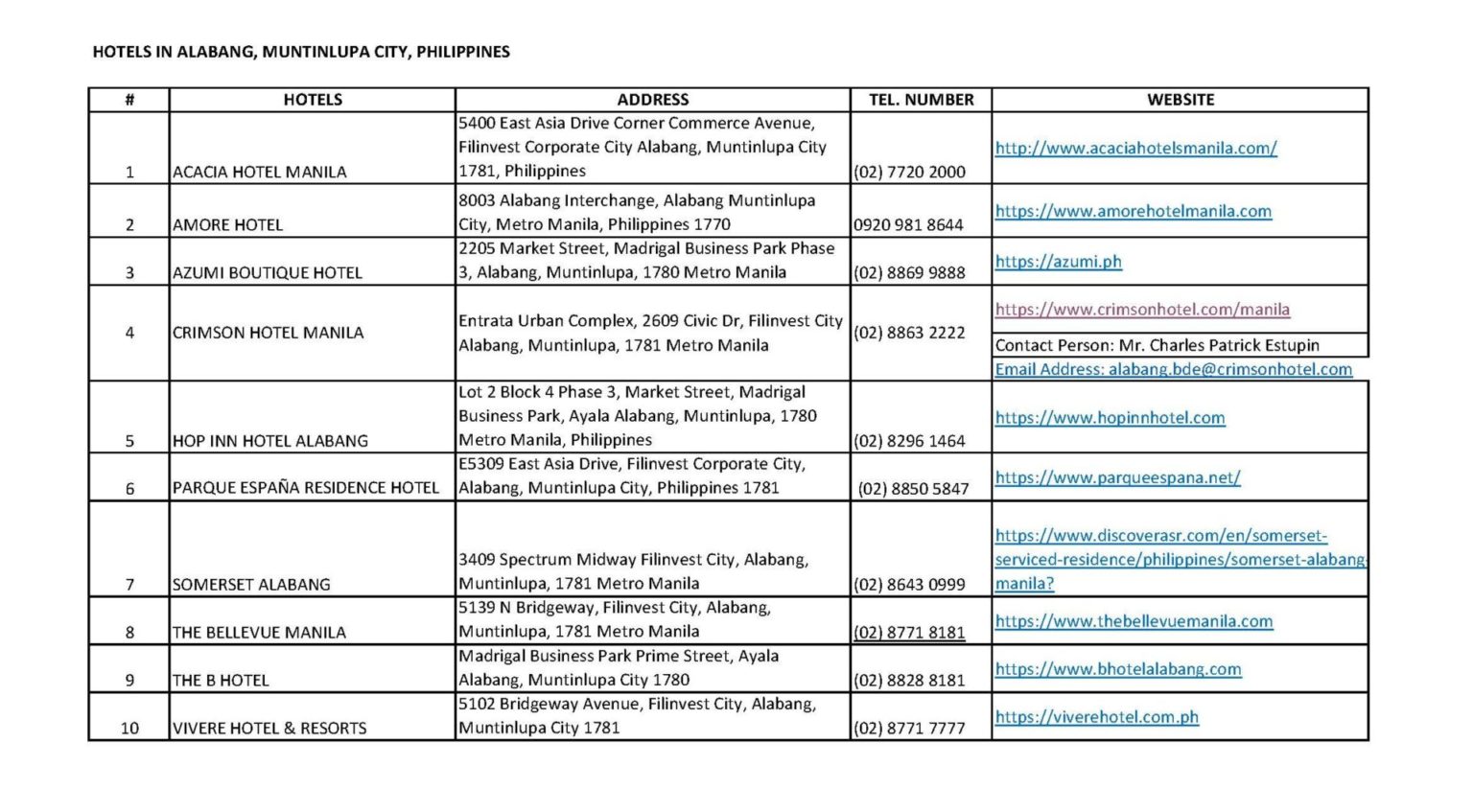
Accommodation
Click here to download the PDF version.